The majority of Australians need the power to register as organ and tissue donors when renewing or making use of for his or her driver’s licence, new analysis exhibits.
Six in 10 respondents to a YouGov ballot had been in favour of getting this energy – which is supported by the nation’s Organ and Tissue Authority – with backing rising to 71 per cent amongst Baby Boomers.
Only South Australian residents at the moment have this selection and DonateLife figures present the state has the nation’s highest registration fee of 72 per cent. Seven in 10 SA households are additionally saying ‘yes’ to their family members turning into donors when requested in hospital.
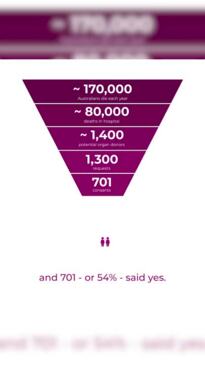
These figures are nicely above the nationwide averages of 36 per cent for registration and 54 per cent for household consent.
The OTA aimed to have 50 per cent of individuals aged 16-plus on the Australian Organ Donor Register and a 70 per cent nationwide consent fee in 5 years’ time, chief government Lucinda Barry stated.
This would lead to an estimated 300 extra individuals per 12 months receiving lifesaving and life-changing organ transplants.
“To achieve that, we need to make sure people can register easily,” Ms Barry stated. “The evidence from SA shows one way of achieving that is through driver’s licences.”
In 2022, 1224 Australians obtained organs from 454 donors.
Fifty-seven per cent of respondents to the ballot of 1025 individuals had been additionally in favour introducing an opt-out system the place all individuals are presumed to consent to organ and tissue donation, until they specify in any other case.
Changes like these are being thought-about in Victoria and Western Australia, because the states undertake parliamentary inquiries into the effectiveness of the present system.
The OTA – which has offered submissions to each inquiries – says an opt-out system wouldn’t be a “silver bullet” for enhancing donations.
“The perception that opt-out means there would be thousands more donors (is) not true,” Ms Barry stated.
“Only 2 per cent of people who die in Australian hospitals die in a way they can be considered for donation. In 2022, that was only 1400 people.
“And regardless of whether we’re opt-in or opt-out, families will always be asked to consent to donation. In opt-out systems across the world (including in Spain and the UK), if the family objects, donation won’t proceed.”
OTA nationwide medical director and senior intensive care specialist Helen Opdam stated for households requested to consent to donation, figuring out their cherished one needed to be a donor was “incredibly important”.
“The big problem is families not knowing what their relatives wanted,” Associate Professor Opdam stated. “Having a system where people can easily opt in, such as through their driver’s licences, is so helpful to that conversation.”
All 4 UK nations have launched opt-out programs over the previous eight years, whereas retaining the power for individuals to opt-in.
Representatives of the UK’s National Health Service informed Victoria’s parliamentary inquiry this week that the nations had been nonetheless seeing vital opt-in registrations – as much as one million a 12 months – following the change.
Assistant director for organ donation John Richardson stated the primary UK nation to introduce opt-out, Wales in 2015, launched the brand new system with a “comprehensive media campaign and household mail drop”. Wales’ household consent fee elevated within the years to comply with, however Covid had since negatively impacted consent throughout the UK.
“Potential organ donors who have an opt-in registration still represent our highest rate of consent, about 90 per cent,” he stated.
“The bulk of our opt-ins come from people renewing their drivers’ licences (73 per cent in 2022).”
The YouGov ballot additionally reveals seven in 10 Australians mistakenly imagine not everybody can register to be a donor – significantly those that have had most cancers, smoke or drink or are typically unhealthy – and three in 10 don’t know how you can register.
“It doesn’t matter how old or unhealthy you are,” Dr Opdam stated. “Anyone aged 16 and above, please register and leave it up to the health professionals to determine whether you’re suitable to become a donor.”
Australians can register at donatelife.gov.au or by way of the Medicare app.
samantha.landy@news.com.au
From transplant child to gold medallist
The change in nine-month-old Anthony Schiller after his liver transplant was nearly instantaneous.
His swollen stomach went down and the yellow jaundiced tinge to his pores and skin and in his eyes went away.
The child, who hadn’t even been capable of roll over but and who had little or no urge for food, was rolling backward and forward in his cot and serious about meals by the point he left Melbourne’s Royal Children’s Hospital.
It was a pleasure for Tanunda mother and father Louise and Cameron Schiller, who had watched their little boy battle since being born with biliary atresia, a blockage within the ducts of the liver.
“In the first eight hours after surgery, Anthony had a bleed, so he had to go back into surgery to find the source. But after that, he came around in leaps and bounds,” Mrs Schiller stated. “By the time he was discharged, you would never have known he was sick a day in his life.”
Every week after his biliary atresia prognosis, Anthony had his first surgical procedure to attempt to save his liver. It was unsuccessful, so he was positioned on the organ donor waitlist. Within three months, a match was discovered.
While he had missed a couple of early developmental milestones, the toddler quickly made up for his gradual begin. He was strolling by 19 months, his language growth progressed quickly and his poor muscle tone was quickly a distant reminiscence as he threw himself into swimming and Little Athletics.
In April, four-year-old Anthony was the youngest competitor on the World Transplant Games in Perth, competing in a dash race, shot put-like “ball throw” and lengthy bounce, incomes gold and silver medals.
“He met so many people from around the world,” Ms Schiller stated. “International athletes were teaching him how to start at the starting blocks and he was having a ball interacting with them all.
“He’s a happy, normal little kid who has been given this amazing gift.”
Family celebrates Mia’s second and third possibilities at life
Mia Geise was “full of life straight away” after her second liver transplant.
It has been nearly a 12 months because the 11-year-old discovered the liver she had obtained as a child had “packed it in”. Fortunately, on the identical day, her mother and father had been informed a brand new organ had been discovered for her.
“She was back at school six weeks later,” stated her dad, Michael Geise. “Her teachers and everyone were so overwhelmed by how good she looked.
“She was back in the pool for swim training, doing squads. We have been careful managing the reintroduction of other activities, but she will also go back to dance this term, which is great.
“Before this transplant, Mia was feeling very unwell and struggling to do even routine stuff. In the 18 months leading up to it, she’d had to give up dance, drama and music.
“It’s fantastic to see how well she is doing now.”
Mia obtained her first transplant 4 months after she was born with liver failure. The Toowoomba lady suffered points all through the ten years with that organ, however she has been luckier the second time round.
Mr Geise stated he, Mia’s mum, Annie, and 13-year-old brother Henry had been grateful each day for the 2 items which have allowed their little lady a second and third likelihood at life.
“As a family, we celebrate yearly on the date of her first liver transplant,” he stated. “Without that first liver, Mia wouldn’t be here.
“We think of that donor and their family often. We also received a letter from the second donor’s mother, it was very heartfelt and I think it was important for her to know Mia was travelling well. We also share the grieving she has for the passing of her son.”
The Geise household urges others to register for organ and tissue donation.
“You’re never too young or too old to have organs that can help to improve the life of someone – or even save a life,” Mr Geise stated.
Sydney dad feels a ‘real connection’ to coronary heart donor
Jayden Cummins thought he had contracted the worst flu ever when he went to the chemist for over-the-counter remedy in 2017.
One take a look at the Camperdown man and his pharmacist informed him to go to his GP, who found he had a really quick irregular coronary heart fee. She despatched him straight to hospital the place it was found he was struggling extreme cardiomyopathy, or end-stage coronary heart failure.
At St Vincent’s Hospital in Darlinghurst, Mr Cummins’ situation deteriorated and he was positioned on a life-supporting extracorporeal membrane oxygenation machine.
The final phrases he remembers saying to his sister had been, “please look after my boy”, referring to his then-13-year-old son, Henry.
Mr Cummins awoke from a coma three weeks later with a mechanical coronary heart.
“For 436 days, I literally wore my heart on my sleeve,” the filmmaker joked concerning the synthetic coronary heart that quickly changed his broken organ, and which was powered by a transportable machine he carried exterior his physique.
“I was so glad to be alive. I wanted to do BridgeClimb but they wouldn’t let me, so I climbed Mt Kilimanjaro with my cousin and a mate. It took us nine hours and I cried all the way up there, I was so appreciative.”
Mr Cummins went on the organ donor waitlist in May 2018 and obtained his new coronary heart 9 months later.
He awoke the day after his surgical procedure feeling “a million bucks” and with a brand new lease on life.
He has continued to embrace an lively life, finishing the City2Surf and the 28km 7 Bridges Walk, and profitable the Anytime Fitness National Success of the Year award in 2018. He additionally received engaged to girlfriend Sanda Bowing after his transplant.
“I think about the person whose heart I have every single day, without fail,” he says. “I even talk to him.
“I feel like I’m the guardian of this heart, it’s not mine, it’s his, and I feel a real connection with him.”
From nightly dialysis to dancing, swimming and a traditional life
Ruby England has been a “completely different child” since receiving a brand new kidney, her grandmother says.
Donna England will always remember the phrases the physician uttered 5 years in the past, when she took her then-four-year-old granddaughter to hospital on the recommendation of her physician: “she has end-stage kidney failure”.
Ruby would generally complain she was drained and get up with a swollen face, however her physician would dismiss these signs as being attributable to a virus once they rapidly disappeared every time.
A wierd bruise on Roby’s chest in the end triggered the physician to ship her straight to hospital, the place blood exams revealed kidney failure.
“It was the worst night. To hear those words about a little girl who up until then had been like any normal child was rough,” stated Ms England, who had been Ruby’s carer most of her life, alongside husband Craig. “I spent the night crying my eyes out.”
Ruby instantly had a tube inserted into her tummy so she may start dialysis.
Every night time for a 12 months, she was hooked as much as a dialysis machine from 7pm to 7am, even when it was her birthday or Christmas. This dominated out sleepovers or occurring faculty camps. Even baths and showers had been a difficult impediment, as her tube needed to keep dry and sterile.
Almost a 12 months to the date that Ruby was placed on the organ transplant waitlist, an ideal kidney match was discovered for her. She had the surgical procedure in January 2021 and it wasn’t lengthy earlier than she was up and about.
Of the now nine-year-old, Ms England stated: “She loves dancing and has singing lessons, she has such a very sweet voice. And she loves her swimming lessons and cooking.
“As a family (which includes Ruby’s brothers, Connor, 16 and Ashton, 13) we always remember that Ruby has this life because of the gift from the donor.”
Darwin girl’s post-pregnancy transplant a lifesaver
Three months after the beginning of her second little one, Efronsi Soula Yiannakos was recognized with a uncommon blood dysfunction that in the end landed her on the organ transplant waitlist.
The 38-year-old Darwin resident was informed she had atypical haemolytic uraemic syndrome (aHUS), a one-in-a-million nightmare triggered by her being pregnant.
Ms Yiannakos had already suffered from Type 1 diabetes because the age of 5. Her aHUS, which causes blood clots to type within the kidneys, led to kidney failure and weeks of hospitalisation, dialysis and plasma change.
With a new child daughter and four-year-old son at residence, Ms Yiannakos spent seven weeks in hospital coming to phrases with life on the transplant waitlist.
“It was devastating, I couldn’t be home to look after my daughter, or my son who was constantly asking ‘when’s mum coming home?’” Ms Yiannakos stated.
For 22 months, she endured three-day-a-week dialysis classes whereas navigating bodily and emotional challenges.
After 11 months on the waitlist, Ms Yiannakos underwent a profitable kidney and pancreas transplant in Sydney, releasing her from dialysis and insulin dependency whereas granting a second likelihood at a satisfying life.
“My diabetes was well controlled with insulin and there was no evidence of the diabetes anywhere else in my body but the pancreas,” she stated.
“The minute I had the transplants, my body took to them so well that I didn’t have to have the insulin, I didn’t have to do dialysis again.”
As Australia’s organ and tissue donation program maintains strict confidentiality, stopping well being professionals from disclosing any data that would determine donors or recipients, Ms Yiannakos won’t ever know who her donor was.
“I can’t thank them and their family enough,” she stated.
“It’s hard to express because you don’t know these people, they’re complete strangers and they want to help others in a time where they’re grieving the most.
“I would still be on dialysis and I wouldn’t be well at all (without them). You don’t last forever on dialysis.”
Source: www.news.com.au